All too often I am asked the question… Have I got Sciatica? Well what really is sciatica? Lets go through a brief anatomy lesson first:
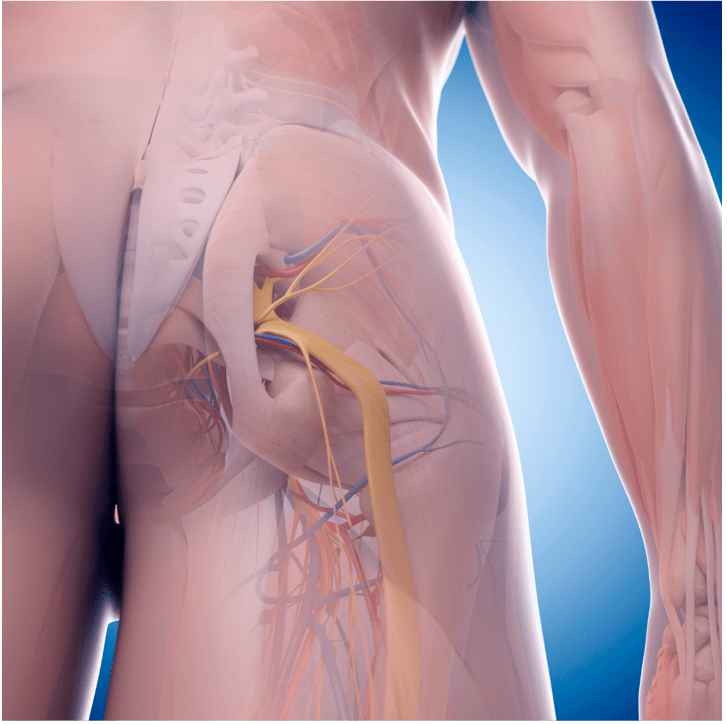
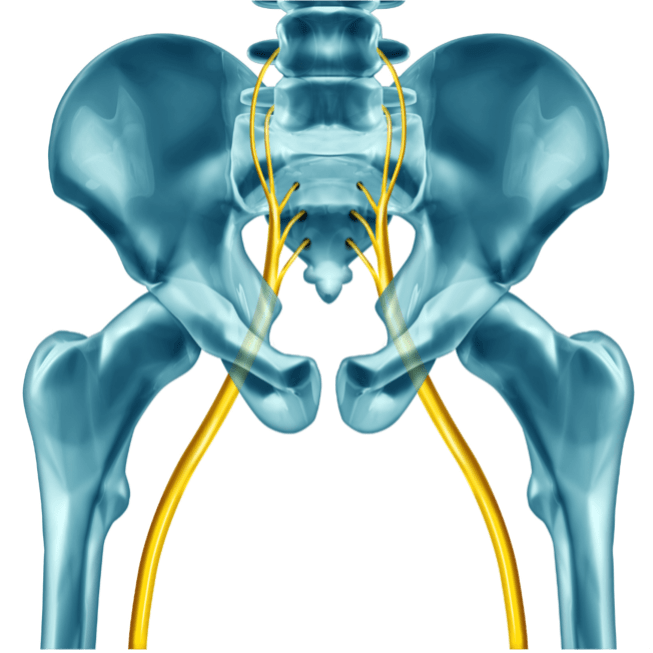
Firstly the sciatic nerve is a VERY large nerve – in fact the longest and thickest nerve in the body, one on either side. It is made up of 5 spinal nerve roots L4, L5, S1, S2 S3 that unite in the pelvis to become the sciatic nerve. The only true sciatic nerve entrapment is generally due to direct trauma into the pelvis such as a hip dislocation or fracture in the hip area, or surgical trauma such as hip replacement surgery intramuscular injection or even radiation treatment. However it must be stressed that these medical causes are VERY RARE.
So what have patients got when they think they’ve trapped their sciatic nerve……
Usually it is one or more of the spinal nerve roots that make up the sciatic nerve that becomes irritated, inflamed, pinched or compressed that then gives patients the sciatica picture or pain running down, usually the back of the leg, which may or may not be accompanied by tingling, numbness and sometimes even weakness into the foot or lower leg.
So let’s look at some of the myths
1. Sciatica is a diagnosis in itself:
The medical definition for sciatica is the pain that radiates down the leg, often caused by compression or irritation of the sciatic nerve. It’s a symptom, not a diagnosis in itself. The underlying cause such as acute of chronic disc issues, spinal stenosis degenerative facet problems or even piriformis syndrome needs to be addressed.
2. Sciatica can’t be cured:
While severe sciatica may require surgery in some cases, a majority of people experience relief with conservative treatments like osteopathy, physiotherapy, acupuncture, rehabilitation, medication, and lifestyle modifications. There is a very small subgroup of people who even after manual therapy, medication and even surgery, still suffer with some degree of discomfort.
3. Bed rest is the answer:
The only time bed rest is the answer is when someone has a ragingly acute disc prolapse and they simply cannot move. However, for the vast majority a combination of structural activity combined with short periods of rest is by far the better solution along with movements or exercises that have been prescribed by your trained healthcare practitioner. Bed rest in these less acute cases can actually worsen sciatica and slow recovery. Motion is lotion is generally the order of the day.
4. Sciatica is caused my piriformis syndrome:
Piriformis is a muscle that is deep in the pelvis and the sciatic nerve passes behind it. The thinking on piriformis syndrome (sometimes called Deep Gluteal Syndrome) is that as the piriformis muscles tightens is can irritate, trap or inflame the sciatic nerve, causing pain down the back of the leg and tenderness in the buttock. Unfortunately, these are also classic symptoms of those of a lumbar spinal nerve being irritated. Just because it’s felt in the glute, doesn’t mean the source of the problem is the glute. I think many cases where people think it’s their piriformis are it is simply referred from the lumbar spine. But you could say it’s a real ‘pain in the bum’!
So if you want to know more about sciatic pain, we have many practitioners here at the Centre For Complementary Health, please get in touch.